Show Notes
Episode Overview:
Introduction to HypernatremiaDefinition and basic conceptsClinical presentation and risk factorsDiagnosis and management strategiesSpecial considerations and potential complications
Definition and Pathophysiology:
Hypernatremia is defined as a serum sodium level over 145 mEq/L.It can be acute or chronic, with chronic cases being more common.Symptoms range from nausea and vomiting to altered mental status and coma.
Causes of Hypernatremia based on urine studies:
Urine Osmolality > 700 mosmol/kgCauses:Extrarenal Water Losses: Dehydration due to sweating, fever, or respiratory lossesUnreplaced GI Losses: Vomiting, diarrheaUnreplaced Insensible Losses: Burns, extensive skin diseasesRenal Water Losses with Intact AVP Response:Diuretic phase of acute kidney injuryRecovery phase of acute tubular necrosisPostobstructive diuresis
Urine Osmolality 300-600 mosmol/kgCauses:Osmotic Diuresis: High glucose (diabetes mellitus), mannitol, high ureaPartial AVP Deficiency: Incomplete central diabetes insipidusPartial AVP Resistance: Nephrogenic diabetes insipidus
Urine Osmolality < 300 mosmol/kgCauses:Complete AVP Deficiency: Central diabetes insipidusComplete AVP Resistance: Nephrogenic diabetes insipidus
Urine Sodium < 25 mEq/LCauses:Extrarenal Water Losses with Volume Depletion: Vomiting, diarrhea, burnsUnreplaced Insensible Losses: Sweating, fever, respiratory losses
Urine Sodium > 100 mEq/LCauses:Sodium Overload: Ingestion of salt tablets, hypertonic saline administrationSalt Poisoning: Deliberate or accidental ingestion of large amounts of salt
Mixed or Variable Urine SodiumCauses:Diuretic Use: Loop diuretics, thiazidesAdrenal Insufficiency: Mineralocorticoid deficiencyOsmotic Diuresis with Renal Water Losses: High glucose, mannitol
Risk Factors:
Patients with impaired thirst response or those unable to access water (e.g., altered or ventilated patients) are at higher risk.Important to consider underlying conditions affecting thirst mechanisms.
Diagnosis:
Initial assessment includes history, physical examination, and laboratory tests.Key tests: urine osmolality and urine sodium levels.Lab errors should be considered if the clinical picture does not match the lab results.
Management Strategies:
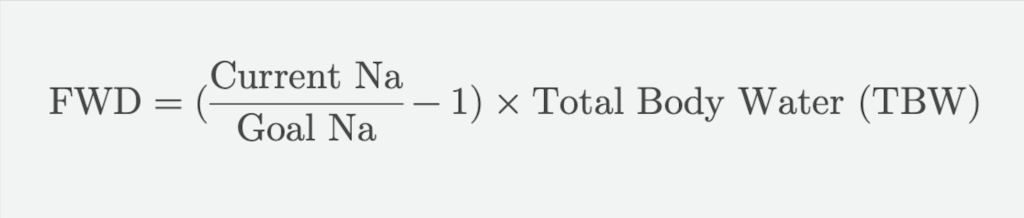
Calculate the Free Water Deficit (FWD) to guide treatment.
Administration routes include oral, NGT, G-tube, or IV with D5W for larger deficits.Safe correction rate is 10-12 mEq/L per day or 0.5 mEq/L per hour to avoid cerebral edema.Address hypovolemia with isotonic fluids before correcting sodium.
Monitoring and Follow-Up:
Monitor sodium levels every 4-6 hours.Assess urine output and adjust free water administration as needed.Admission to ICU for symptomatic patients or those with severe hypernatremia (sodium >160 mEq/L).Decision to discharge vs admit is a complicated one that factors in symptoms, etiology, degree of hypernatremia, patient preference, access to follow up, etc.
Take Home Points:
Hypernatremia is a serum sodium level over 145 mEq/L, with symptoms ranging from nausea to coma.It is primarily caused by water loss exceeding intake due to various factors like sweating, vomiting, diarrhea, and renal issues.Correcting hypernatremia too quickly can lead to cerebral edema, so a safe correction rate is essential.Initial treatment involves calculating the Free Water Deficit and selecting the appropriate administration route.Monitor sodium levels frequently and decide on admission or discharge based on symptoms, sodium levels, and patient’s ability to follow up.
